Unified data layers solve a critical issue in multi-clinic healthcare: fragmented patient information. Despite widespread adoption of Electronic Health Records (EHRs), data silos prevent seamless sharing of patient histories, lab results, and treatment plans across locations. This lack of integration leads to incomplete reporting, inefficiencies, and compliance risks.
Unified data systems integrate scattered data into a single structure, enabling centralized access and real-time reporting. By using standards like FHIR and TEFCA, these systems ensure secure and accurate data sharing. The result? Faster reporting, reduced errors, and better compliance with regulations like the 21st Century Cures Act.
Key benefits include:
- Improved data accuracy: Eliminates duplicate records and resolves inconsistencies.
- Centralized reporting: Provides real-time insights across all clinic locations.
- Enhanced decision-making: Supports faster diagnoses and streamlined workflows.
Scimus offers custom integration services, QA testing, and scalable enterprise solutions to help healthcare networks unify their data systems. This approach reduces inefficiencies, strengthens reporting, and improves patient care across multi-clinic organizations.
Healthcare Data Fragmentation: Costs and Benefits of Unified Systems
Problems with Fragmented Data in Multi-Clinic Healthcare
Data Silos and Reporting Barriers
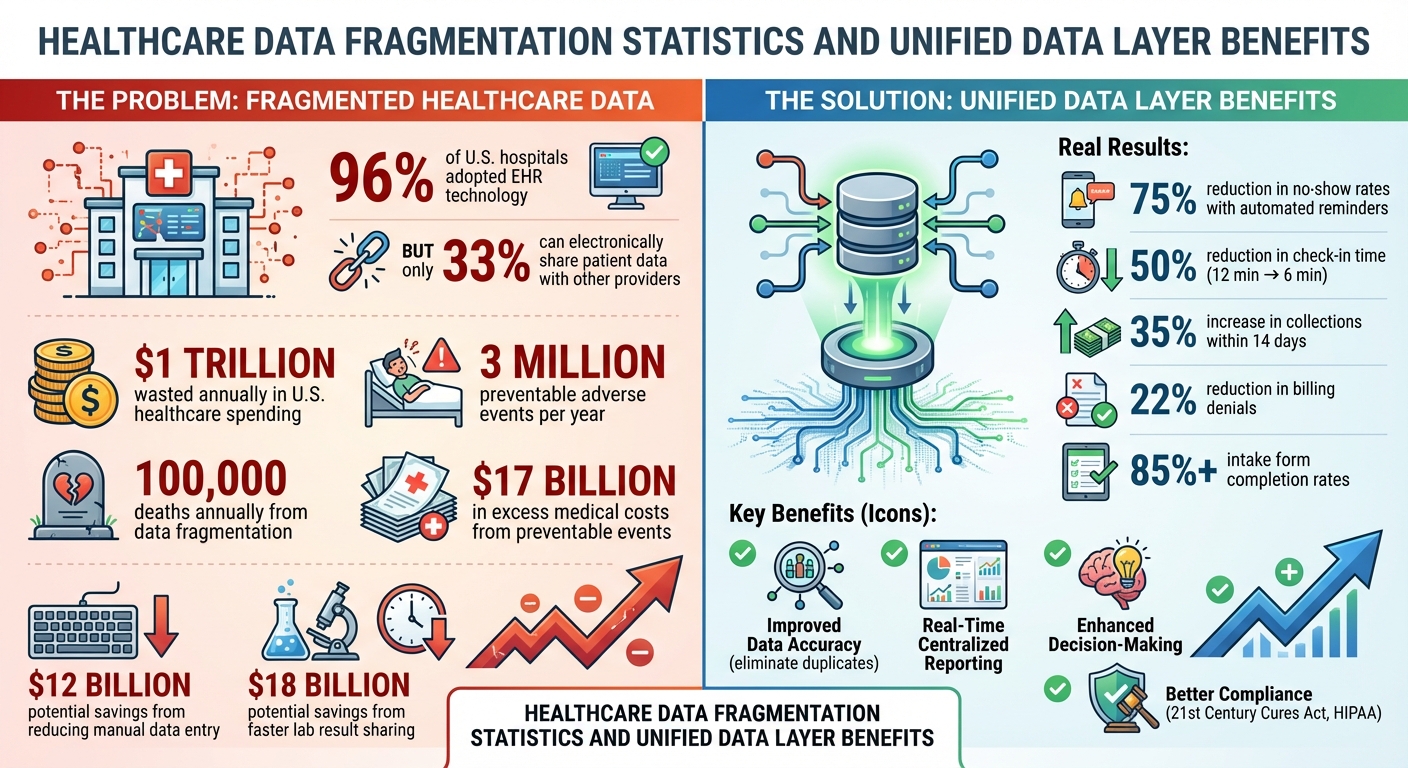
Fragmented data systems pose a major challenge for multi-clinic healthcare organizations trying to produce accurate and comprehensive reports. While 96% of hospitals and 78% of physicians' offices in the U.S. had adopted certified EHR technology by 2016, fewer than one in three hospitals could electronically locate, send, receive, and integrate patient data from another provider. This disconnect stems from the fact that many EHR systems rely on proprietary data formats, making seamless communication difficult.
These silos lead to inefficiencies that burden clinical staff with extra manual tasks, such as entering vital signs from devices into patient charts. This process is not only time-consuming but also expensive. For instance, reducing the time clinicians spend on manual data entry could save the healthcare sector $12 billion annually. Additionally, faster sharing of critical information like lab results could trim hospital stays and save another $18 billion each year.
"The lack of integration common throughout health care would be unacceptable on safety grounds alone in any other high-risk field."
The National Academy of Medicine draws attention to how industries like aviation, telecommunications, and banking have embraced standardized systems - think ATM cards or universal phone chargers - driven by consumer demand. In contrast, healthcare has lagged in pushing for consistent interoperability. These inefficiencies don’t just hinder operations; they also amplify compliance risks, which we’ll explore next.
Compliance and Regulatory Risks
The fragmented systems caused by data silos create significant compliance challenges, especially for multi-clinic organizations. These gaps in seamless information exchange directly conflict with the requirements of the 21st Century Cures Act of 2016. This legislation mandates that health IT systems must enable secure, effortless exchange of electronic health information while ensuring full access to all legally accessible data.
The consequences of these inefficiencies are dire. Fragmented systems contribute to an estimated 3 million preventable adverse events annually, resulting in $17 billion in excess medical costs and nearly 100,000 deaths each year. The National Academy of Medicine has warned that delaying the adoption of interoperable systems not only heightens legal exposure but also increases economic risks tied to avoidable errors.
Interoperability at scale: Technical strategies for health data integration
How Unified Data Layers Work: Architecture and Components
Unified data layers tackle the challenges of fragmented healthcare data by creating a foundation for seamless multi-clinic reporting. These systems bring together data from various sources into a single platform, simplifying how clinics handle reporting across multiple locations. The architecture consists of three key layers - source, storage, and presentation - that work together to collect, organize, and analyze data efficiently.
Here’s how these layers interact: the source layer gathers raw data from different healthcare systems, the storage layer organizes and secures this information in a central repository, and the presentation layer turns it into actionable insights through dashboards and reports. Additional layers ensure data security, compliance, and governance, safeguarding sensitive patient information and meeting regulations like HIPAA.
Let’s dive deeper into how each layer contributes to unifying healthcare data.
Source Layer: Connecting Different Data Systems
The source layer acts as the bridge between fragmented systems, pulling data from Electronic Health Records (EHRs), lab systems, radiology platforms, billing systems, wearable devices, and IoT technologies. Using an API-first approach, it employs pre-built connectors and tools for data validation and cleaning right at the start. This setup includes ingestion endpoints, real-time change capture tools, and self-service options that allow users to add new data sources without heavy IT involvement.
To ensure smooth communication between incompatible systems, the source layer relies on industry standards like HL7, FHIR (Fast Healthcare Interoperability Resources), and DICOM. These standards harmonize data formats, making it easier for systems to exchange information. Once the data is cleaned and validated, it moves to a secure, centralized repository.
Storage Layer: Central Data Repository
The storage layer serves as the backbone for securely storing healthcare data, whether it’s structured data like patient demographics or unstructured information like clinical notes and medical images. Organizations typically use data lakes, warehouses, or lakehouses to store both raw and processed data.
This centralized repository streamlines access for authorized users across the network while incorporating backup and disaster recovery features to protect against data loss. By maintaining data integrity and ensuring compliance with retention policies, the storage layer lays the groundwork for delivering reliable insights.
Once organized, the data moves to the presentation layer for analysis and visualization.
Presentation Layer: Real-Time Reporting Access
The presentation layer transforms raw and aggregated data into meaningful insights through tools like dashboards, reporting interfaces, and mobile apps. These tools visualize information in the form of charts, graphs, and other user-friendly formats. For multi-clinic organizations, this layer provides a unified, continuously updated view of operations and patient care across different systems.
For instance, clinicians can access customizable charts that display personalized patient summaries or clinical cards at the point of care. This real-time access empowers both healthcare professionals and executives to make informed decisions quickly - critical in situations where time is of the essence.
Benefits of Unified Data Layers for Multi-Clinic Reporting
When healthcare organizations with multiple clinics bring scattered data together into a single, unified system, they can improve patient care, simplify operations, and strengthen compliance with regulations. This approach tackles common challenges like incomplete patient records, duplicated efforts, and compliance risks. It also lays the groundwork for comprehensive, actionable reporting across all clinic locations.
Improved Data Accuracy and Compliance
A unified data layer ensures accurate and consistent patient information by eliminating duplicate records and resolving conflicting data. Advanced algorithms match details such as name, date of birth, gender, and Social Security Number, ensuring providers access up-to-date and reliable clinical data. Any discrepancies are flagged for review, allowing healthcare professionals to focus on accurate and consistent information rather than piecing together fragmented records.
Quicker Reporting with Centralized Access
With a unified data layer, reporting becomes faster and more efficient. Centralized access provides a full, real-time view of patient information across all specialties and care settings, enabling quicker diagnoses and timely treatment adjustments. This system ensures the right information is available precisely when needed, which is critical for proactive patient care. For administrators, centralized dashboards track key operational metrics, making it easier to measure performance, identify areas for improvement, and demonstrate ROI with clear data. By consolidating data into a single source of truth, healthcare organizations can generate accurate reports instantly.
Enhanced Decision-Making and Operational Efficiency
Unified data access empowers clinics to close care gaps, reduce redundancies, and speed up billing processes. This not only supports faster and safer decision-making but also improves overall efficiency. With a complete view of patient data, providers can make more informed clinical decisions, leading to quicker diagnoses, better communication with patients, and safer care delivery. Ultimately, having accurate and accessible information drives better decisions, which translates into superior patient outcomes and more streamlined clinic operations.
sbb-itb-116e29a
Implementation Strategies with Scimus Services

Bringing a unified data layer to multi-clinic healthcare networks is no small feat. It requires precise integration, thorough quality checks, and reporting systems that can scale effortlessly. Scimus steps in with a strategic approach to tackle fragmented systems and deliver dependable reporting solutions.
Custom Data Integration and Development
Data fragmentation can be a major roadblock in healthcare networks. Scimus addresses this by creating tailored integration solutions that link disconnected healthcare data systems. Their method involves building robust data pipelines that extract, clean, and standardize data from various sources. The result? Smoother workflows and simplified reporting processes.
QA and Automation Testing for Data Pipelines
Data integrity is non-negotiable, especially in healthcare. To ensure accuracy, Scimus implements strict quality assurance protocols. Automated validation rules are embedded into the data exchange process, catching errors before they can impact reporting outcomes.
Enterprise Solutions for Scalable Reporting
Managing data across large, multi-clinic networks requires advanced solutions. Scimus creates enterprise-grade reporting systems by leveraging data lakes for raw data storage and data warehouses for structured insights. Their architecture supports both day-to-day operational reporting and long-term analytics, all while complying with healthcare standards like USCDI, FHIR, and TEFCA. This ensures the system remains accurate, compliant, and scalable across the entire network.
Results from Unified Data Layers in Healthcare
Case Study: Multi-Clinic Network Reporting Optimization
Unified data layers have shown real, measurable benefits. For example, a pediatrics group tackled long check-in times by linking mobile intake forms directly to their EMR system. The results? Check-in times dropped from 12 minutes to just 6, with over 75% of patients completing their forms before arriving.
In another case, a family medicine practice resolved billing inefficiencies that were causing revenue losses. By syncing digital intake forms with their EMR, they cut billing denials by 22% within three months. Even better, intake form completion rates surpassed 85%, meaning staff spent less time chasing incomplete paperwork.
A multi-specialty group turned its attention to collections. By adding automated billing reminders through their communications platform, they saw a 35% increase in collections within 14 days.
These examples highlight how operational improvements pave the way for even greater performance gains, as seen in the benchmarks below.
Performance Metrics and Benchmarks
Unified data layers not only improve workflows but also deliver strong performance metrics. For instance, automated appointment reminders integrated with EMR schedules can cut no-show rates by up to 75%. This means fewer empty slots and better use of resources across clinics.
Workflow automation also reduces duplicate data entry and errors, which lowers claim denials and frees staff to focus on patients. Accurate data leads to fewer medication mistakes and less unnecessary testing, improving both patient safety and outcomes.
The financial benefits are hard to ignore. With around $1 trillion wasted annually in U.S. healthcare spending, much of it due to poor data sharing, unified data layers address a critical issue. Faster billing cycles, streamlined intake processes, and better compliance all contribute to stronger financial health for multi-clinic networks.
Conclusion
Fragmented systems drain multi-clinic organizations of billions of dollars through lost revenue, inconsistent data, and countless wasted staff hours. These challenges call for a solution that not only addresses inefficiencies but also streamlines operations.
By integrating EHRs, labs, imaging systems, billing platforms, and communication tools, unified data layers tackle these issues head-on. They eliminate duplicate entries, reduce inconsistencies, and speed up reporting cycles. The result? More accurate data, improved compliance with regulations, and fewer manual tasks. Plus, they provide real-time insights that empower better decision-making across entire networks.
Scimus steps in with tailored integration services, QA automation, and scalable enterprise solutions to help healthcare organizations turn fragmented data into meaningful, actionable insights. By solving the unique reporting challenges that multi-clinic systems face, Scimus helps these organizations unlock the full potential of their data - enhancing patient care and driving operational efficiency.
Unified data layers aren't just a technological upgrade - they're a game-changer in how healthcare systems manage and utilize information.
FAQs
How can unified data layers help healthcare organizations stay compliant with regulations?
Unified data layers bring together scattered clinical, financial, and operational data into one standardized system. This ensures consistent terminology across the board and eliminates discrepancies. By centralizing data, healthcare organizations gain a clear, audit-ready trail detailing who accessed or modified records, along with the when and why - critical for meeting HIPAA and other regulatory standards.
These systems are built on nationally recognized frameworks like USCDI and HL7 FHIR, ensuring that stored data aligns with federal reporting requirements from agencies like CMS and HRSA. By automating data extraction and reducing manual errors, unified data layers simplify the creation of accurate, regulator-mandated reports. This not only saves time but also helps avoid costly compliance penalties, allowing healthcare providers to concentrate on what truly matters - delivering quality care.
What makes up a unified data layer in multi-clinic healthcare systems?
A unified data layer in healthcare consolidates scattered clinical, operational, and financial data into a single, dependable source. It typically includes several essential components:
- Data integration pipelines: These gather information from systems like electronic health records (EHRs), lab systems, and billing platforms. They rely on frameworks such as the United States Core Data for Interoperability (USCDI) and FHIR to standardize and harmonize the data.
- Centralized storage system: Often implemented as a cloud-based data lake or warehouse, this system is designed to store both raw and processed data efficiently, offering scalability and cost-effectiveness.
- Governance layer: This ensures data quality, manages access policies, and enforces compliance with regulations like HIPAA.
- API layer: This component allows real-time access to unified data for reporting tools and analytics systems.
- Analytics tools: Dashboards or AI models transform the unified data into actionable insights, enabling better decision-making.
By integrating these components, healthcare organizations can simplify reporting, enhance data accuracy, and ensure compliance with healthcare regulations across multiple clinics.
How do unified data layers enhance efficiency in multi-clinic healthcare systems?
Unified data layers serve as a hub for combining clinical, financial, and operational data across an entire clinic network. By standardizing information and breaking down data silos, these systems help eliminate errors from inconsistent coding or duplicate entries. This means easier access to accurate patient records, appointment schedules, and billing details, which not only simplifies workflows but also allows staff to dedicate more time to patient care.
Since the data is already standardized and stored in one place, generating reports becomes quicker and more seamless. Executives can produce performance dashboards, regulatory reports, and financial summaries without the hassle of manually collecting and cleaning data from different sources. Unified data layers also enhance compliance efforts by maintaining consistent audit trails, ensuring adherence to HIPAA and state regulations, and making inspections less complicated.
Cloud-based systems take this a step further by offering scalable analytics tools and real-time decision-making capabilities. For multi-clinic networks, this translates into better operational efficiency, cost savings, and the ability to deliver higher-quality care backed by data-driven insights.

